Creating Mixed Simulation Training During a Pandemic
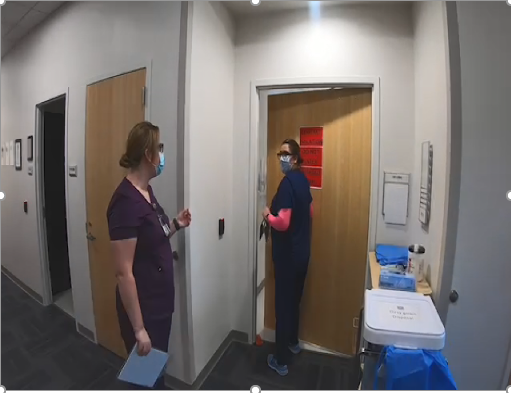


Photos: (Top Left) Hannah Bailey (left) and Nativity Sullins (right), Stop the line when another staff member is not following guidelines to use PPE. (Top Right) Michael Lewis (left) Hannah Bailey (near door) and Nativity Sullins (near window), stop the line when medication administration and patient identification is not clear. (Bottom Center) Nativity Sullins (left) and Anna Lumba (right), when needed the situation may need to be elevated to the nurse manager to Stop the Line. Photos courtesy of Bonnie Barti.
By: Bonnie Barti, MAed., Simulation Technician, VA Southern Nevada Healthcare System
Faced with a mandate to create and teach simulation training during a pandemic, there are multiple hurdles simulation centers must overcome to successfully meet new constraints. In January 2021, our education staff was tasked to develop training based on the Stop the Line for Patient Safety, the (STLPS) program applies to all nursing staff while maintaining social distancing and safety protocols. “Stop the Line” is a VA-wide initiative that empowers VHA employees to speak up immediately if they see a risk to patient safety. Launched in 2013, this awareness campaign encourages employees to report behaviors, action, or inaction that might result in errors or patient harm (Department of Veterans Affairs, 2015). The timeline included 30 days to create the training and 60 days to train a minimum of 90% of inpatient registered nurses.
Our educators developed new methodologies to create simulations under pandemic restrictions. With limited access to in-situ environments, simulation laboratory rooms and classroom settings, we shifted to a mix of limited in person sessions with prerecorded simulation following the standards of best practice established by the International Nurses Association for Clinical Simulation and Learning (INACSL). The team modified the simulation modality, pre-brief and debrief techniques to reduce potential viral exposure. The project was created and maintained within Microsoft Teams, with all members able to add, review, delete or discuss parts of the training.
The simulation educators first created pre-session assignments using Elsevier's Clinical Skills to prepare learners for the activity. A Microsoft PowerPoint presentation formed the basis of the STLPS training combined with pre-recorded and embedded simulated patient scenarios. The scenarios were scripted and to provide the learners an opportunity to see three instances where they could “stop the line.” Three staff members played the roles of the nursing staff and patient for the scenarios. Three simulation scenarios were chosen, including entering and isolation room without Personal Protective Equipment (PPE), medication administration error and blood transfusion patient identification error. The video scenarios were shown to the participants to analyze the situation and state how they would handle the concern using the 3 “W” model. The 3 “W” model is: Say what you see; Say what you are concerned about; and, Say what you want to happen to keep things safe (AHRQ, n.d.). Simulation Educators were able to play, pause and debrief the video content with a similar style as they would if the simulation was live and participants were able to physically participate.
As the Simulation Technician, the focus was on modality and fidelity. The simulation scenarios were captured on video via VA purchased GoPro, then edited in a free app iMovie (Apple). The finished product was then uploaded into free app YT studio in YouTube from the device. From YT studio, the video was able to be uploaded to Microsoft Teams or to the Microsoft PowerPoint presentation.
Creating simulation training during the pandemic required a change in our educational paradigms and techniques. By embracing technology and suspending reality through video-recorded simulation scenarios, training was accomplished safely and timely. The advantages of mixed simulation include standardized training, reliable and consistent information provided to learners, and availability of courses. Further simulation trainings have been created following the STLPS to include Morse Fall Scale (AHRQ, n.d.), and Go Training (first 5 minutes of a code; many VAMCs use this training). Future trainings could be held completely virtual via Microsoft Teams meeting now that instructors better understand how to use the technology to complete courses virtually with embedded recorded simulation scenarios.
References:
Foronda, C. L. (2021). What is virtual simulation? Clinical Simulation in Nursing, 52, 8. https://doi.org/10.1016/j.ecns.2020.12.004
Home. INACSL. (n.d.). Retrieved September 22, 2021, from https://www.inacsl.org/.
Kuszajewski, M. L., Vaughn, J., Bowers, M. T., Smallheer, B., Hueckel, R. M., & Molloy, M. A. (2021). Embracing disruption: Measuring effectiveness of virtual simulations in advanced practice nurse curriculum. Clinical Simulation in Nursing, 57, 41–47. https://doi.org/10.1016/j.ecns.2021.04.017
Luctkar-Flude, M., & Tyerman, J. (2021). The rise of virtual simulation: Pandemic response or enduring pedagogy? Clinical Simulation in Nursing, 57, 1–2. https://doi.org/10.1016/j.ecns.2021.06.008
Luctkar-Flude, M., Tyerman, J., Verkuyl, M., Goldsworthy, S., Harder, N., Wilson-Keates, B., Kruizinga, J., & Gumapac, N. (2021). Effectiveness of debriefing methods for virtual simulation: A systematic review. Clinical Simulation in Nursing, 57, 18–30. https://doi.org/10.1016/j.ecns.2021.04.009
Peachey, L., McParland, T., Goldsworthy, S., & Williams, V. (2021). P stands for pivot: Pivoting face-to-face practicum to virtual simulation during the pandemic. Clinical Simulation in Nursing, 57, 53–58. https://doi.org/10.1016/j.ecns.2021.04.021
Tool 3H: Morse fall scale for identifying fall risk factors. AHRQ. (n.d.). Retrieved September 22, 2021, from https://www.ahrq.gov/patient-safety/settings/hospital/fall-prevention/toolkit/morse-fall-scale.html.
US Department of Veterans Affairs, V. H. A. (2015, March 11). Va.gov: Veterans Affairs. Stop the Line for Patient Safety Initiative. Retrieved September 22, 2021, from https://www.qualityandsafety.va.gov/stoptheline/stoptheline.asp.



















